Professor Christian Flotho
E: christian.flotho@uniklinik-freiburg.de
T: (00) 49 (0)761 270 46 280
F: (00) 49 (0)761 270 46 282
Medical Center – University of Freiburg
Center for Pediatrics
Department of Pediatric Hematology and Oncology
Mathildenstraße 1
79106 Freiburg
Germany
Juvenile myelomonocytic leukemia (JMML) is a malignant myeloproliferative disorder of early childhood. The central aim of our research is the elucidation of the early epigenetic dynamics in JMML through integrated global and focal DNA methylation profiling, transcriptome analysis and mass spectrometric proteomics, both in patient-derived xenograft models and in primary clinical material.
TEAM
- Dr. rer. nat. Zoé Wehbe (Postdoc)
- Dr. rer. nat. Foued Ghanjati (Postdoc)
- Dr. rer. nat. Khaled Alatibi (Postdoc)
- Melanie Guimaraes Moreira (Technician)
- Marlou Schoof (MD student)
RESEARCH THEMES
JMML is an aggressive mixed myeloproliferative/myelodysplastic neoplasm that occurs mainly in young children. Although allogeneic hematopoietic stem cell transplantation (HSCT) is still the mainstay of successful therapy, it is associated with considerable toxicity and a high risk of failure. Accordingly, we aim to understand the mechanisms regulating treatment resistance and relapse of the disease.
Our previous studies have confirmed the involvement of epigenetic mechanisms in the etiopathogenesis of JMML. The most common epigenetic alteration involves cytosine hypermethylation at 5‘ genetic regions, already considered a hallmark of high-risk JMML. The efficacy of the DNA methyltransferase inhibitor azacitidine for treatment of JMML was demonstrated and confirmed in a multicenter, international, phase 2 clinical trial (AZA-JMML 001, registered as a Pediatric Investigation Plan with the European Medicines Agency; EudraCT 2014‐002388‐13 and NCT 02447666), for which our institution provided central medical coordination, reference diagnostics, and pharmacodynamic studies. In an ancillary study to this trial, we focus on understanding the early cellular effects of DNA hypomethylation in JMML by integrating DNA methylation profiling, transcriptome analysis, and mass-spectrometry proteomics. We anticipate that the characterization of disordered global and focal DNA methylation and its consequences will contribute to better diagnosis and management of JMML.
The nature of JMML-initiating cells, the cellular hierarchy, and the clonal architecture of the malignant cells remain poorly characterized. Our current work addresses the role of intratumoral clonal diversity in disease progression and treatment resistance in JMML. We hypothesize that the early presence of cell subpopulations that give rise to therapy-resistant cell clones is a key factor determining the risk of progression or relapse and hence the ultimate outcome. While previous characterization of the genetic landscape in JMML was based on bulk leukemic cell samples, we now create genetic maps at the single-cell level in samples from a well-documented patient cohort and associate these with hematologic and clinical information.
To expand the possibilities of modeling the disease for translational research, we reprogram induced pluripotent stem cells (IPSCs) from JMML bone marrow cells of various genotypes and epigenotypes and redifferentiate these cells into hematopoietic lineages. This will allow using the lines for preclinical testing of novel therapeutic principles, for example substances targeting the leukemic cell metabolism at the level of oxidative phosphorylation.
SELECTED RECENT PUBLICATIONS
-
Wu Y, Zehnle PMA, Rajak J, Koleci N, Andrieux G, Gallego-Villar L, Aumann K, Boerries M, Niemeyer CM, Flotho C, Bohler S, Erlacher M. BH3 mimetics and azacitidine show synergistic effects on juvenile myelomonocytic leukemia. Leukemia. 2024 Jan;38(1):136-148. doi: 10.1038/s41375-023-02079-5. Epub 2023 Nov 9. PMID: 37945692; PMCID: PMC10776398.
-
Ramamoorthy S, Lebrecht D, Schanze D, Schanze I, Wieland I, Andrieux G, Metzger P, Hess M, Albert MH, Borkhardt A, Bresters D, Buechner J, Catala A, De Haas V, Dworzak M, Erlacher M, Hasle H, Jahnukainen K, Locatelli F, Masetti R, Stary J, Turkiewicz D, Vinci L, Wlodarski MW, Yoshimi A, Boerries M, Niemeyer CM, Zenker M, Flotho C. Biallelic inactivation of the NF1 tumour suppressor gene in juvenile myelomonocytic leukaemia: Genetic evidence of driver function and implications for diagnostic workup. Br J Haematol. 2023 Nov 9. doi: 10.1111/bjh.19190. Epub ahead of print. PMID: 37945316.
-
Vinci L, Flotho C, Noellke P, Lebrecht D, Masetti R, de Haas V, De Moerloose B, Dworzak M, Hasle H, Güngör T, Starý J, Turkiewicz D, Ussowicz M, de Heredia CD, Buechner J, Jahnukainen K, Kallay K, Bodova I, Smith OP, Zecca M, Bresters D, Lang P, Masmas TN, Meisel R, Pichler H, Erlacher M, Göhring G, Locatelli F, Strahm B, Niemeyer CM, Yoshimi A. Second allogeneic stem cell transplantation can rescue a significant proportion of patients with JMML relapsing after first allograft. Bone Marrow Transplant. 2023 May;58(5):607-609. doi: 10.1038/s41409-023-01942-4. Epub 2023 Feb 23. PMID: 36823455; PMCID: PMC10162940.
-
Wehbe Z, Ghanjati F, Flotho C. Induced Pluripotent Stem Cells to Model Juvenile Myelomonocytic Leukemia: New Perspectives for Preclinical Research. Cells. 2021 Sep 6;10(9):2335. doi: 10.3390/cells10092335. PMID: 34571984; PMCID: PMC8465353.
-
Mayerhofer C, Niemeyer CM, Flotho C. Current Treatment of Juvenile Myelomonocytic Leukemia. J Clin Med. 2021 Jul 13;10(14):3084. doi: 10.3390/jcm10143084. PMID: 34300250; PMCID: PMC8305558.
-
Niemeyer CM, Flotho C, Lipka DB, Starý J, Rössig C, Baruchel A, Klingebiel T, Micalizzi C, Michel G, Nysom K, Rives S, Schmugge Liner M, Zecca M, Schönung M, Baumann I, Nöllke P, Benettaib B, Biserna N, Poon J, Simcock M, Patturajan M, Menezes D, Gaudy A, van den Heuvel-Eibrink MM, Locatelli F. Response to upfront azacitidine in juvenile myelomonocytic leukemia in the AZA-JMML-001 trial. Blood Adv. 2021 Jul 27;5(14):2901-2908. doi: 10.1182/bloodadvances.2020004144. PMID: 34297046; PMCID: PMC8341358.
-
Schönung M, Meyer J, Nöllke P, Olshen AB, Hartmann M, Murakami N, Wakamatsu M, Okuno Y, Plass C, Loh ML, Niemeyer CM, Muramatsu H, Flotho C, Stieglitz E, Lipka DB. International Consensus Definition of DNA Methylation Subgroups in Juvenile Myelomonocytic Leukemia. Clin Cancer Res. 2021 Jan 1;27(1):158-168. doi: 10.1158/1078-0432.CCR-20-3184. Epub 2020 Nov 2. PMID: 33139265; PMCID: PMC7785676.
-
Niemeyer CM, Rudelius M, Shimamura A, Flotho C, Hasle H, Stieglitz E, Strahm B, Godley LA, Weinberg OK, Orazi A, Calvo KR. Classification of rare pediatric myeloid neoplasia-Quo vadis? Leukemia. 2022 Dec;36(12):2947-2948. doi: 10.1038/s41375-022-01731-w. Epub 2022 Oct 21. PMID: 36271151.
- Niemeyer C.M. and Flotho C. (2019) Juvenile myelomonocytic leukemia: who’s the driver at the wheel? Blood 133, 1060-1070. DOI: 10.1182/blood-2018-11-844688
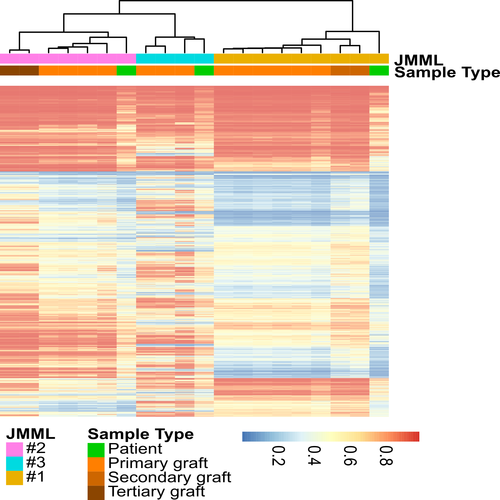
- Krombholz C.F., Gallego-Villar L., Sahoo S.S., Panda P.K., Wlodarski M.W., Aumann K., Hartmann M., Lipka D.B., Daskalakis M., Plass C., Niemeyer C.M., Erlacher M. and Flotho C. (2019) Azacitidine is effective for targeting leukemia-initiating cells in juvenile myelomonocytic leukemia. Leukemia 33, 1805-1810. DOI: 10.1038/s41375-018-0343-2
- Lipka D.B., Witte T., Toth R., Yang J., Wiesenfarth M., Nollke P., Fischer A., Brocks D., Gu Z., Park J., Strahm B., Wlodarski M., Yoshimi A., Claus R., Lubbert M., Busch H., Boerries M., Hartmann M., Schonung M., Kilik U., Langstein J., Wierzbinska J.A., Pabst C., Garg S., Catala A., De Moerloose B., Dworzak M., Hasle H., Locatelli F., Masetti R., Schmugge M., Smith O., Stary J., Ussowicz M., Van Den Heuvel-Eibrink M.M., Assenov Y., Schlesner M., Niemeyer C., Flotho C.* and Plass C.* (2017) RAS-pathway mutation patterns define epigenetic subclasses in juvenile myelomonocytic leukemia. Nat Commun 8, 2126. (*jointly supervised this work). DOI: 10.1038/s41467-017-02177-w
- Krombholz C.F., Aumann K., Kollek M., Bertele D., Fluhr S., Kunze M., Niemeyer C.M., Flotho C.* and Erlacher M.* (2016) Long-term serial xenotransplantation of juvenile myelomonocytic leukemia recapitulates human disease in Rag2-/-gammac-/- mice. Haematologica 101, 597-606. (*contributed equally to this work). DOI: 10.3324/haematol.2015.138545
- Cseh A., Niemeyer C.M., Yoshimi A., Dworzak M., Hasle H., Van Den Heuvel-Eibrink M.M., Locatelli F., Masetti R., Schmugge M., Gross-Wieltsch U., Candas A., Kulozik A.E., Olcay L., Suttorp M., Furlan I., Strahm B. and Flotho C. (2015) Bridging to transplant with azacitidine in juvenile myelomonocytic leukemia: a retrospective analysis of the EWOG-MDS study group. Blood 125, 2311-2313. DOI: 10.1182/blood-2015-01-619734
COLLABORATIONS, CO-OPERATIONS AND NETWORKS
FUNDING
- DFG Collaborative Research Center 992 “Medical Epigenetics”
- BMBF consortium “MyPred” (Information in German)